This is the ultimate guide For Temporomandibular Joint Syndrome. In this blog, we have covered what is TMJ? Classification of TMJ, Sign & symptoms of TMJ, Diagnosis, and Treatment for TMJ.
WHAT IS TEMPOROMANDIBULAR JOINT SYNDROME (TMJ) ?
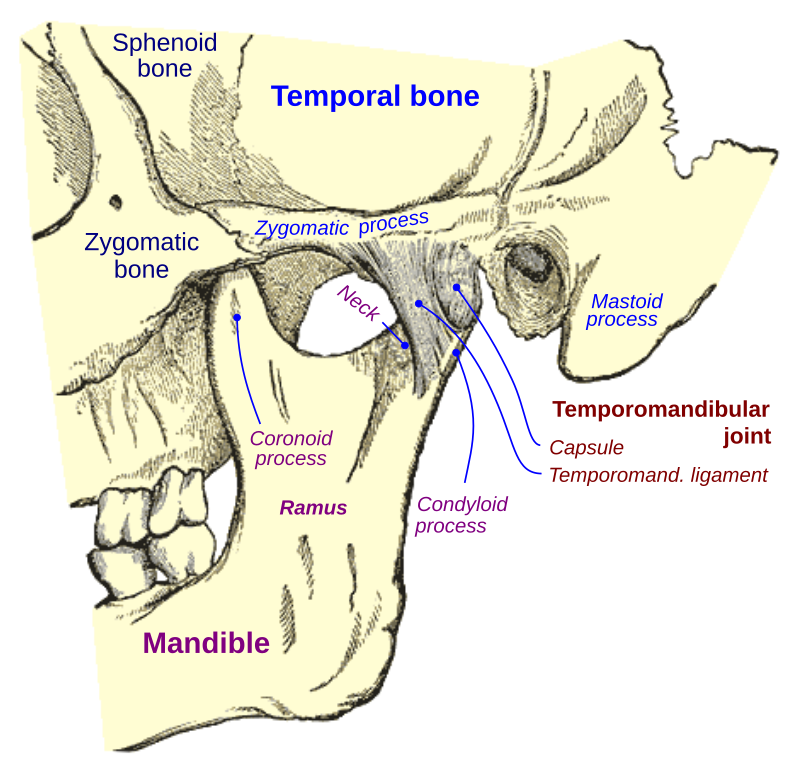
- Temporomandibular joint and muscle disorders, also commonly known as “TMJ”, it is a conditions that cause pain and dysfunction in the jaw joint and the muscles that control jaw movement.
- Temporomandibular joint (TMJ) problems affect large properties of the population at one time or another.
- Women are more likely to significant from TMJ problems than men.
- Temporomandibular joint problems often have significant psychological, as well as physical causes.
Image Source & Credit Jmarchn – Own work, CC BY-SA 3.0, Link
CAUSES OF TMJ :
- Trauma
- Malocclusion
- Teeth grinding
- Stress or anxiety
- Arthritis or inflammatory musculoskeletal disorders
- Orthodontic braces
- Excessive gum chewing
- Hormonal
- Genetic
CLASSIFICATION OF TMJ :
- Developmental disorder of joint
- Inflammatory joint disease
- Traumatic disorder of TMJ
- Degenerative joint disease
- Metabolic disorder
- Neoplastic disorder
- Myofascial pain dysfunction syndrome
- Osteoarthritis
- TMJ dislocation
- Disc displacement with or without reduction
SIGN AND SYMPTOMS :
- Pain or tenderness in the jaw (either at rest or when eating).
- Aching pain in-ear or around the ear.
- Difficulty in chewing or pain while chewing.
- Aching facial pain
- Locking of the jaw
- Difficult to open or close the jaw.
- Limited mandibular opening.
- History of trauma or infection.
- Earache.
- Clicking, popping or grinding sounds of the temporomandibular joints.
- Dull ache in face and neck
- Headache (maybe worse in the morning)
- Limitation in jaw opening
- Swelling and increase temperature over muscles
- Inflammation in the tendentious attachment of the muscles
DIAGNOSIS:
Doctor will discuss the symptoms and examine jaw:
- Press on the area around jaw to identify the sites of pain or discomfort
- Listen to feel your jaw when you open and close your mouth
- Observe the range of motion in your jaw
- A localized, constant muscles pain secondary to trauma, infection,or overuse of a muscle.
TREATMENT:
No stronge evidence exists to suggest the single best treatment for Temporomandibular joint disorders.
Treatment planning should involve balancing the patient’s wishes with potential risks and benefits of treatment.
- STEP 1: Patient education and self-care.
- STEP 2: behavioral modification.
- identify the specific problem.
- Cognitive-behavioral self-regulation exercise. Physical therapy referral.
- STEP 3 : Pharmacotherapy
- Analgesic.
- Muscle relaxants.
- Tricyclic Antidepressant.
- STEP 4: Trigger point management.
- Injection with local anesthetic
- Physical therapy: vapocoolant spray or ice application and stretching.
- STEP 5: Orthopedic appliance therapy -muscle relaxation splint
- STEP 6: Surgical procedure:
- Arthrocentesis
- TMJ arthroscopy Modify colotomy
- Modify colotomy.
- Open joint surgery
- RADIOLOGY :
- MRI: For joint space pathology
- CT: For bony pathology
- OTHERS :
- Occlusal adjustments and orthodontics.
- open surgery
BENEFITS OF LASER TREATMENT FOR TMJ :
- Acceleration healing and reduce long-lasting pain.
- Simple and comfortable application of infrared light.
- No heat is omitted it will not damage cells or burns the skin or surrounding tissues.
- No side effect.
- Can be used in all ages
- Help improve movement and physical function.
- Noninvasive and nonsurgical treatment.
- It can improve the health of your damage jaw disk as well as speed up your recovery time.
- Laser therapy assists blood flow thus increase oxygen, glucose, and nutrient.
- Reduce free radicals and oxidation stress.
- Increase cell metabolism
- And healing the nerve surrounding the jaw.
- Dry surgical field and better visualization, less bleeding.
- Tissue is kept sterilized, cleaned and thus less number of bacteria.
- Decreased swelling, edema and scarring.
- Less pain.
- Faster healing response
- Increased patient acceptance.
- Minimal mechanical trauma.
- Not harmful to eyes and skin, as protective eyewear’s are used.
- No requirement of sutures.
- Reduce surgical time.
- Advantage for medically compromised patients.
- No medication is required like antibiotics or pain killers.
- The patient becomes free of fear and anxiety.
- Hemostatic effect by sealing blood vessels.
- Minimal damage to surrounding tissues.
- No irritating sound like traditional drills.