dental pulp pdf, dental pulp stem cells, dental pulp removal, type of nerve fibers in dental pulp, tooth pulp exposed, pulp chamber, nerve supply of pulp, tooth pulp infection
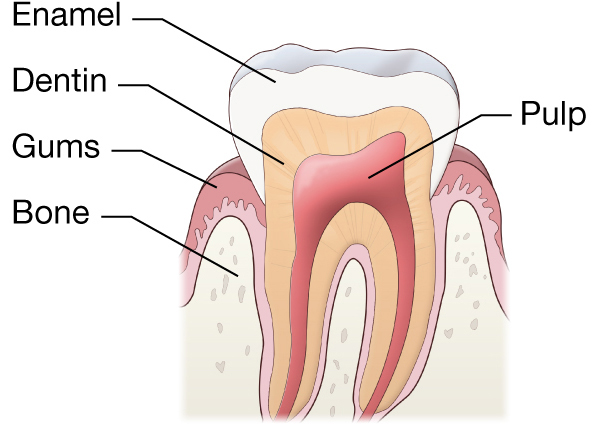
Dental Pulp is the soft connective tissue that occupies the pulp cavity in the central part of the teeth.
Causes of Dental Pulp-
In Human teeth, there are enamel and dentin layers that protect the pulp from bacterial infection.diseases of dental pulp occur when these two protective layers are damaged or breakdown and bacteria begin to multiply within the pulp chamber. Different causes of Dental Pulp are as follows:
1. Physical Causes of dental pulp Disease:
- Mechanical:
- Accidental or iatrogenic dental procedures.
- Pathological wear.
- Crack through the body of the tooth
- Thermal:
- Heat prone cavity preparation-
- Electrical:
- Electronic pulp testers
2. Chemical Causes of dental pulp Disease:
- Erosion or phosphoric acid.
3. Bacterial Causes of dental pulp Disease:
- Toxin associated with caries.
- Direct invasion of pulp from caries or trauma or by some blood-borne microorganisms.
Types of Pulp Diseases:
Reversible Pulpitis:
It is a mild to moderate inflammatory condition of the pulp by noxious stimuli. In which pulp is capable of returning to uninflamed state once by removal of the stimuli.
Tooth is sensitive to thermal changes, especially cold.
Irreversible pulpitis
it is a persistent inflammatory condition of the pulp, symptomatic or asymptomatic, caused by noxious stimuli. It may be acute or chronic.
Most Common Sites of Occurrence
- Primary and permanent teeth
- Sites of recent or defective restorations
- Sites of recent trauma
Signs
Reversible pulpitis
- Caries
- Exposed dentin
Irreversible pulpitis
- Deep caries
Symptoms
Reversible pulpitis
- Non-lingering pain to temperature or osmotic changes
Irreversible pulpitis
- Intense, lingering pain to temperature changes
- Spontaneous pain
- Diffuse or referred pain
Investigation
- Obtain thorough dental history and inquire about recent restorations or trauma.
- Inquire about the previous history of pain on the offending tooth.
- Ask the patient about:
a. Location of the offending tooth
b. When did the pain start?
c. How intense is the pain?
d. What causes the pain and what relieves it?
e. How long does the pain last?
f. Pain description (e.g., dull, sharp, throbbing)
- Perform an intraoral examination to check for exposed dentin, caries, a deep or defective restoration, or trauma.
- Perform a percussion test to rule out acute apical periodontitis.
- Perform a cold test using a refrigerant spray (e.g., Endo-Ice®) or an ice stick. Test the healthy control teeth first in order to better localize the offending tooth.
- Perform a hot test using hot water in a syringe (e.g., Monojet®) and rubber dam isolation, a heated gutta-percha stick or heat source (e.g., System B™ Heat Source) to reproduce pain to hot. Healthy control teeth should be tested first. Delayed and prolonged pain triggered by heat may indicate irreversible pulpitis.
- Use radiographs to identify teeth with large restorations or caries that are not clinically visible. Keep in mind that teeth with reversible or irreversible pulpitis will not show periapical lesions radiographically, but may show thickening of the periodontal ligament (PDL), loss of lamina dura, and/or condensing osteitis. Irreversible pulpitis may show widened PDL space.
Diagnosis
Based on clinical examination and testing, a diagnosis of reversible or irreversible pulpitis is determined.
Reversible Pulpitis
- Pain from cold test does not linger more than 30 s
- No percussion sensitivity
- No spontaneous pain
- No heat sensitivity
Irreversible Pulpitis
- Pain from cold test lingers more than 30 s
- May get pain from heat test
- May have spontaneous pain
- Maybe percussion sensitive
- Radiographically or clinically visible deep caries
Differential Diagnosis
Pain of non-odontogenic origin:
- Musculoskeletal pain
- Neurovascular pain
- Neuropathic pain
- Pain caused by a distant pathology (cardiovascular, cranial, throat, neck)
- Psychogenic pain
Treatment
Common Initial Treatments
Reversible pulpitis
- Remove the irritant or repair tooth structure (caries, exposed dentin, defective restoration).
- Continue to monitor the patient’s symptoms.
- Advise patient to return if symptoms persist or worsen.
Irreversible pulpitis
- Pulpectomy of the offending tooth: complete removal of the pulp. If it is determined that the case in question is too complex, promptly refer to an endodontist.
- If treatment is undertaken and the appointed treatment time permits, root canal treatment can be completed in one visit.
Antibiotics are not recommended for irreversible pulpitis as they will not alleviate the patient’s pain and should not be given in lieu of performing an immediate pulpectomy.
Alternate Treatments
Perform extraction
Chronic Hyperplastic Pulpitis It is also called as pulp polyp It is a productive pulpal inflammation due to extensive carious exposure of a young pulp.
HISTOLOGIC FEATURES: The T surface of the pulp polyp is usually covered by the stratified squamous epithelium. Such epithelium may be derived from the gingiva or from freshly desquamated epithelial cells of mucosa and tongue. T granulation tissue is young, vascular connective he tissues containing polymorph nuclear neutrophils, lymphocytes, and plasma cells.
Stratified sq. epithelium covering polyp
CAUSES
Slow, progressive carious of the pulp is the cause. F development of hyperplastic pulpitis, a large, open or cavity a young resistant pulp, and chronic, low-grade stimulus are necessary. Mechanical irritation from chewing or bacterial infection often provide the stimulus. symptoms It is symptomless, except during mastication, when the pressure of food bolus may cause discomfort.
TREATMENT PROGNOSIS: Extraction of tooth or pulp extirpation.
Internal resorption
It is an idiopathic slow or fast progressive resorption process occurring in the dentin of the pulp chamber or root canals of teeth.
Histopathology
It is a result of osteoclast activity
There is resorptive process is characterized by lacunae, which may be by osteoid tissue.
PULP POLYP
Multinucleated giant cell dentinoclast are present. Metaplasia of pulp. Causes
It is unknown but maybe there is a history of trauma.
Symptoms
In the root of a tooth is asymptomatic.
In crown, it may be manifested as a reddish area called “pink spot”. Diagnosis
It is diagnosed during routine radiographic examination.
The appearance of the “pink spot” occurs late in he resorptive process when the integrity of the crown has been compromised.
radiograph usually shows a change in the appearance he of the wall in the root canal or the pulp chamber, with a round or ovoid radiolucent area.
Treatment and prognosis
Routine endodontic treatment is indicated , obturation of the defect requires a special effort UT ,preferred with a plasticized gutta-percha method . When root is perforated, then mineral trioxide aggregate (MTA) is used to repair. prognosis is favorable before perforation of the root he or crown occurs.
PULP DEGENERATION
Pulp degeneration is usually present in teeth of old people. It may also result in persistent, mild irritation in the teeth of young patients.
1.Calcific degeneration :
In calcific degeneration part of the pulp tissue is replaced by calcific material i.e., stone or denticles. It may occur in root canal or pulp chamber. The calcific material has a limitation structure, like the he skin of an onion, and lies unattached within the body of
2. Atrophic degeneration
In this type, observed histopathological in pulp of older people, Fewer stellate cells are present and intercellular fluids is increased. pulp tissue is less sensitive than normal.
3. Fibrous degeneration
In this type, the pulp is characterized by the replacement of the cellular elements by fibrous connective tissue. On removal of root canal, such pulp has the characteristic appearance of leathery fibrous.
NECROSIS OF PULP
It is the death of the pulp. It may be partial or total, depending on whether part or the entire pulp is involved.
Types:
1. Coagulation
2.Caseation
3.Liquefaction
Causes It can be due to any noxious insult injurious to the pulp, such as bacteria, trauma and chemical irritation.
Clinical features no painful symptoms. discoloration of tooth, tooth is greyish or brownish in color. Pulp is dead.
Management
preparation + obturation of root canals
PROGNOSIS -favourable.
