bump on upper lip,tiny bumps on lips,lip diseases pictures,bump on lip,lip diseases cheilitis,lips colour change disease,eczema on lips
1)DEVELOPMENTAL:
- CONGENITAL LIP PITS
A congenital lip pit or lip sinus is a congenital disorder . They are often hereditary, and may occur alone or in association with cleft lip and palate, termed Van der Woude syndrome.
CLINICAL FEATURES:
- It is more commonly seen in females.
- It is common on vermillion border of either lip and most commonly on the lower lip
- It may be up to 3 to 4 mm in diameter and may extend as deep as 2 cm and communicated with underlying minor salivary glands.
- In some cases, sparse mucus secretion may be visible from the base of the pit.
- Lips sometimes appear swollen accentuating the appearance of the pit.

MANAGEMENT:
Surgical excision for cosmetic purpose.
- COMMISSURAL PITS
A depression located at an oral commissure.
CLINICAL FEATURES:
- It is more common amongst males and black people are affected more than white people.
- Commissural pit appears as a unilateral or bilateral pit at the corner of the mouth on the vermillion surface.
- If it is unilateral, it occurs on the right side of the lip.
- It is localized at angle of mouth with the tract diverging dorsolateral into the cheek.
- Size ranges from a shallow dimple to a tract measuring 4 mm in length and tissue slightly raised above the opening.

MANAGEMENT:
Surgical excision.
- DOUBLE LIP
It is an excess tissue on the inner surface of the lip.
CLINICAL FEATURES:
It is associated with Aschers syndrome which consists of double lip, blepharochalasis (It is drooping of the tissue between eyebrow and edge of the upper eyelid so that it hangs loosely over thyroid enlargement.

MANAGEMENT:
Surgical excision
- CLEFT LIP AND CLEFT PALATE
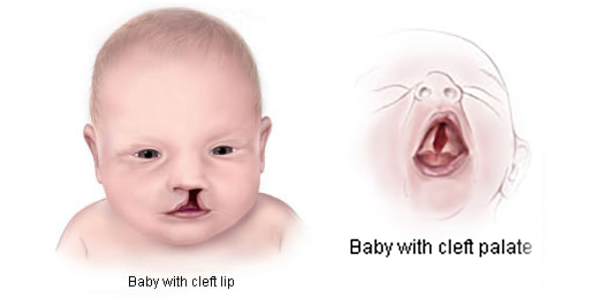
Cleft lip and cleft palate are the most common birth defects. The most commonly occur as isolated birth defects but are also associated with many inherited genetic conditions or syndromes.
cleft lip and cleft palate can be corrected using treatment.
SYMPTOMS:
Usually, a split in the lip or palate is identifiable at birth. Cleft lip and cleft palate appear as:
- A split in the lip that affects both sides of the human face
- A split in the lip that appears as only a small notch in the lip or extends from the lip through the upper gum and palate into the bottom of the nose
Less commonly, a cleft occurs only in the muscles of the soft palate (sub mucous cleft palate), which are at the back of the mouth and covered by the mouth’s lining.
- Difficulty with feedings
- Difficulty swallowing, with potential for liquids or foods to come out the nose
- Nasal speaking voice
- Chronic ear infections.


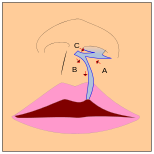

The blue lines indicate incisions.
Movement of the flaps; flap A is moved between B and C. C is rotated slightly while B is pushed down.
CAUSES:
- In most cases, the cause of cleft lip and cleft palate is unknown. These conditions cannot be prevented. Most scientists believe clefts are due to a combination of genetic and environmental factors. There appears to be a greater chance of clefting in a new-born if a sibling, parent, or relative has had the problem.
- Another potential cause may be related to a medication a mother may have taken during her pregnancy. Some drugs may cause cleft lip and cleft palate. Among them: anti-seizure/anticonvulsant drugs, acne drugs containing Accutane, and methotrexate, a drug commonly used for treating cancer, arthritis, and psoriasis.
What Problems Are Associated withCleft Lip and/or Palate?
- Eating problems: With a separation or opening in the palate, food and liquids can pass from the mouth back through the nose. Fortunately, specially designed baby bottlesand nipples that help keep fluids flowing downward toward the stomach are available. Children with a cleft palate may need to wear a man-made palate to help them eat properly and ensure that they are receiving adequate nutrition until surgical treatment is provided.
- Ear infections/hearing loss: Children with cleft palate are at increased risk of ear infections since they are more prone to fluid build-up in the middle ear. If left untreated, ear infections can cause hearing loss. To prevent this from happening, children with cleft palate usually need special tubes placed in the eardrums to aid fluid drainage, and their hearing needs to be checked once a year.
- Speech problems: Children with cleft lip or cleft palate may also have trouble speaking. These children’s voices don’t carry well, the voice may take on a nasal sound, and the speech may be difficult to understand. Not all children have these problems and surgery may fix these problems entirely for some. For others, a special doctor, called speech pathologist, will work with the child to resolve speech difficulties.
- Dental Problems: Children with clefts are more prone to a larger than average number of cavities and often have missing, extra, malformed, or displaced teeth requiring dental and orthodontic treatments. In addition, children with cleft palate often have an alveolar ridge defect. The alveolus is the bony upper gum that contains teeth. A defect in the alveolus can displace, tip, or rotate permanent teeth, prevent permanent teeth from appearing, and prevent the alveolar ridge from forming. These problems can usually be repaired through oral surgery.
TREATMENT:
- A cleft lip may require one or two surgeries depending on the extent of the repair needed. The initial surgery is usually performed by the time a baby is 3 months old.
- Repair of a cleft palate often requires multiple surgeries over the course of 18 years. The first surgery to repair the palate usually occurs when the baby is between 6 and 12 months old. The initial surgery creates a functional palate, reduces the chances that fluid will develop in the middle ears, and aids in the proper development of the teeth and facial bones.
- Children with a cleft palate may also need a bone graft when they are about 8 years old to fill in the upper gum line so that it can support permanent teeth and stabilize the upper jaw. About 20% of children with a cleft palate require further surgeries to help improve their speech.
- Once the permanent teeth grow in, braces are often needed to straighten the teeth.
COMPLICATIONS:

A baby being fed using a customized bottle. The upright sitting position allows gravity to help the baby swallow the milk more easily.
Cleft may cause problems with feeding, ear disease, speech, socialization, and cognition.
Due to lack of suction, an infant with a cleft may have trouble feeding. An infant with a cleft palate will have greater success feeding in a more upright position. Gravity will help prevent milk from coming through the baby’s nose if he/she has cleft palate. Gravity feeding can be accomplished by using specialized equipment, such as the Haberman Feeder, or by using a combination of nipples and bottle inserts like the one shown, is commonly used with other infants. A large hole, crosscut, or slit in the nipple, a protruding nipple and rhythmically squeezing the bottle insert can result in controllable flow to the infant without the stigma caused by specialized equipment.
Individuals with cleft also face many middle ear infections which may eventually lead to hearing loss. The Eustachian tubes and external ear canals may be angled or tortuous, leading to food or other contamination of a part of the body that is normally self-cleaning. Hearing is related to learning to speak. Babies with palatal clefts may have compromised hearing and therefore, if the baby cannot hear, it cannot try to mimic the sounds of speech. Thus, even before expressive language acquisition, the baby with the cleft palate is at risk for receptive language acquisition. Because the lips and palate are both used in pronunciation, individuals with cleft usually need the aid of a speech therapist.
MANAGEMENT:
The complete rehabilitation of the condition requires a multidisciplinary approach.
CHELIOPLASTY: It is surgical closure of the lip. A general rule of tens is used in determining optimal timing of lip closure i.e. 10 weeks of age, 10 pounds of body weight and 10gm of Hb. At the time of lip closure, when an infant is under general anaesthesia an impression is made for the new obturator.
OBTURATOR: Between 3rd and 9th months of age, an obturator is used to provide cross-arch stability support and to prevent collapse of maxillary arch.
PALATOPLASTY: It is performed to close an opening in the palate. Surgeons may close the palate in one surgery when the child is about one year of age or the palate may be closed in two stages the soft palate first followed by the hard palate.
BONE GRAFTING: Sometimes closure of palatal cleft may be done by bone grafting.
ORTHODONTIC THERAPY: To correct malocclusion.
CLEFT RHINOPLASTY: To improve nasal function and correct the distortion.
SPEECH THERAPY
FEEDING PLATE: To overcome initial feeding problems, feeding plate is used which acts as an obturator to prevent nasal reflux.
- CHELITIS
Cheilitis is inflammation of the lips. This inflammation may include the perioral skin (the skin around the mouth), the vermilion border, or the labial mucosa. The skin and the vermilion border are more commonly involved, as the mucosa is less affected by inflammatory and allergic reactions.
CAUSES:
Chronic exposure to sun, wind and dust as well as use of tobacco.
In several cases, emotional disturbances, as well as familial occurrence, suggesting a hereditary pattern.
Inflammation of enlarged heterotopic salivary glands.
A) ANGULAR CHEILITIS:
Angular Cheilitis is a condition that causes red, swollen patches in the corners of your mouth where your lips meet and make an angle. Other names for it are perleche and angular stomatitis. You can get it on one side of your mouth or on both sides at the same time.
SYMPTOMS:
The main things you’ll notice are irritation and soreness in the corner(s) of your mouth. One or both corners may be:
- Bleeding
- Blistered
- Cracked
- Crusty
- Itchy
- Painful
- Red
- Scaly
- Swollen

Your lips can feel dry and uncomfortable. Sometimes your lips and mouth can feel like they’re burning. You also might have a bad taste in your mouth.
If the irritation is strong, it can make it hard for you to eat. You may not get enough nutrients or you may lose weight.
CAUSES:
- Saliva gets trapped and builds up in the corners of your mouth. When it dries, the skin in the area can crack. You may lick your lips often to soothe your cracked skin. The warmth and moisture in the corners of your mouth create the perfect conditions for fungus to grow and multiply — and cause infection.
- Fungal infection is the most common cause of angular Cheilitis. It’s usually caused by a type of yeast called Candida— the same fungus that causes diaper rash in babies. Certain bacteria strains also can cause it.
- If your doctor can’t find the cause, it’s called idiopathic angular Cheilitis.
TREATMENT:
- The goal is to clear out the infection and keep the area dry so your skin isn’t infected again. Your doctor will recommend an antifungal cream to treat fungal infections. Some are:
- nystatin (Mycostatin)
- ketoconazole (Extina)
- clotrimazole (Lotrimin)
- miconazole (Lotrimin AF, Micatin, Monistat Derm)
- If your infection is bacterial, your doctor will prescribe an antibacterial medication, such as:
- mupirocin (Bactroban)
- fusidic acid (Fucidin, Fucithalmic)
- If your angular Cheilitis isn’t caused by a fungal or bacterial infection, your doctor may suggest you put petroleum jelly on the inflamed areas. This protects your mouth from moisture so the sores can heal.
- clear Lift-Clear palate
B)ECZEMATOUS CHEILITIS
Eczematous Cheilitis is inflammation of the lips presenting as redness with dryness and scaling. … The major causes of eczematous Cheilitis are atopic dermatitis and irritant or allergic contact reactions.
CAUSES:
- Lipstick: they are composed of mineral oils and waxes which form the stick; castor oil as a solvent for the dye, lanolin as an emollient preservative, perfumes, and color. The color includes azo dyes and eosin, which is a bromofluorescein derivative.
- Sunscreen applied in the form of lipstick can also cause contact Cheilitis.
- Mouthwashes and dentifrices: Essential oils such as peppermint, cinnamon, clove, spearmint, and bactericidal agents can cause Cheilitis.
- Dental preparations: Mercury and eugenol may cause Cheilitis in the absence of stomatitis. Allergy to epinine containing materials used for crowns and bridges can cause Cheilitis.
- Foods: Oranges, Mangoes and artichokes are among the food plants which occasionally cause allergic Cheilitis and dermatitis of the skin around the lips.
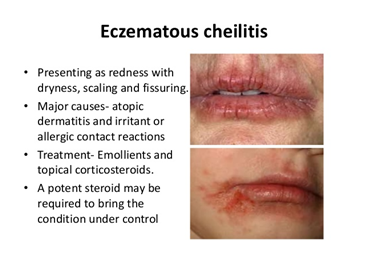
CLINICAL FEATURES:
- The chronic form of eczematous Cheilitis presents with redness, dryness, scaling and fissuring. The angle of the mouth is often also involved (angular Cheilitis).
- The perioral skin and vermilion margin (where the red mucosa meets the skin) are the most commonly affected parts of the lips.
- It is important to look for and note skin and mucosal lesions elsewhere as these may give a clue as to the cause.
TREATMENT:
- Treatment will depend on the cause. Where an exogenous cause has been identified, this should be avoided if possible. If this does not result in improvement, consider another factor such as a second allergen, irritant or endogenous cause.
- For atopic Cheilitis, moisturisers and topical corticosteroids may be recommended.
C) ACTINIC CHEILITIS
- It is also called as actinic keratosis or solar cheilosis.
- It is premalignant squamous cell lesion resulting from long-term exposure to solar radiation and may be found at the vermillion border of lip as well as other sun exposed surfaces.
CLINICAL FEATURES:
- Occurs as the result of sun damage to the lip.
- It is a precancerous condition: squamous cell carcinoma develops in 6-10 per cent of cases.
- Gradual onset of puffiness, with dryness and scaling of the lip that may split and crust. White patches may develop.
MANAGEMENT:
- Topical fluorouracil- for mild cases application 5% fluorouracil 3 times for 10 days.
- Rapid freezing with co2 snow or liquid nitrogen on swab stick is used to remove superficial lesions.
- Biopsy in cases of induration, thickening or ulceration.
- Avoid further sun exposure and advise regular use of sunscreen.
- Imiquimod may be helpful. Cryosurgery or electro surgery may be useful in focal actinic Cheilitis.
- Extensive actinic cheilitis may respond to 5-fluorouracil, carbon dioxide laser or scalpel vermilionectomy.
D)EXFOLIATIVE CHEILITIS
Exfoliative cheilitis is a rare reactive condition presenting as continuous peeling of the lips.
Factitial cheilitis can present as Exfoliative cheilitis, when it is due to attention-seeking or factitial behaviour or an obsessive-compulsive tendency to pick or chap the lips (exfoliative).
CLINICAL FEATURES:
Exfoliative cheilitis presents with continuous peeling of the vermilion (outer) part of the lips. It may affect just one lip, usually the lower. The lip may look normal or red before the formation of the thickened surface layer. The peeling appears to be cyclical and proceeds at different rates in different sites, so there is always some part of the lip peeling at any time. There may be associated bleeding resulting in formation of a haemorrhagic crust. When both lips are involved, the lower lip is usually more affected than the upper.


The condition may be painful, causing difficulty in eating and speaking. Other symptoms reported include sensations of:
- Tingling
- Itch
- Dryness
Ulceration or fissuring may occur.
Depression and personality disorders have been reported commonly in association with factitial exfoliative cheilitis. However, the cheilitis itself can be of such unpleasant appearance that the patient avoids social situations, contributing to mood disturbance.
The typical course of exfoliative cheilitis is chronic over years. It may fluctuate, worsening with further stress. Spontaneous improvement has been reported, but it often recurs.
TREATMENT:
Infection should be treated topically or systemically, if present.
Unless a predisposing or associated condition can be identified and treated, exfoliative cheilitis is typically resistant to treatment. Unsuccessful use of keratolytic lip balms, sunscreen, antifungal creams, topical steroids, systemic steroids, antibiotics, vitamin D analogues(calcipotriol) and cryotherapy have been described. There has been one report each of the successful use of topical tacrolimus and Calendula officinalis (marigold) ointment 10%.
Treatment of an associated mood or anxiety disorder has been reported to improve factitial cheilitis. Obsessive-compulsive disorders respond best to selective-serotonin-reuptake inhibitors.
- GLANDULAR CHELITIS
Glandular cheilitis is a clinical diagnosis. A biopsy of the affected area may be reported as nonspecific. Findings may include: Enlarged salivary glands and ducts. Mixed inflammatory infiltrate.
CAUSES:
The cause of glandular cheilitis is unknown. It is associated with:
- Sun exposure
- Trauma (e.g., lip biting)
- Smoking.
CLINICAL FEATURES:
Cheilitis glandularis typically has the following features:
- Swelling and pouting of the lower lip
- An uneven surface of the lip
- Numerous pin-sized orifices from which saliva can be easily expressed
- Tenderness.


COMPLICATIONS:
- Secondary bacterial infection can result in drainage of pus, ulceration and abscess formation.
- Squamous cell carcinoma may arise, particularly in the context of long term sun exposure and smoking.
MANAGEMENT:
- Vermilionectomy: due to high incidence of associated malignancy a vermilionectomy or surgical stripping of lips has been recommended.
- If lips are grossly enlarged, excision of an elongated ellipse of tissue may be required.
TREATMENT:
In most cases, treatment is not necessary and may be unsuccessful at restoring the lip to normal. In some cases, treatment for associated sun damage or infection may be necessary.
- Topical or oral antibiotics
- Topical or intralesional corticosteroid
- Excision of a nodule suspicious of squamous cell carcinoma
- Vermilionectomy (excision of the entire affected lip)
- GRANULOMATOUS CHEILITIS:
Granulomatous cheilitis refers to an uncommon condition in which there is lumpy swelling of the lips. It is also known as cheilitis granulomatosa or Miescher cheilitis.
CAUSES:
The causes of granulomatous cheilitis include:
- Allergic contact dermatitis
- Crohn disease
- Sarcoidosis
- Orofacial granulomatosis
- Cancer or infection resulting in obstruction of lymphatics around the lips
- A genetic disorder.
SYMPTOMS:
Granulomas in Miescher cheilitis are confined to the lip. In other cases of granulomatous cheilitis, granulomatous disease is more widespread.
The first symptom of granulomatous cheilitis is a sudden swelling of the upper lip. In most cases, this first episode goes away within hours or days. Swelling of the lower lip and one or both cheeks may follow in orofacial granulomatosis. Less commonly, the forehead, eyelids, or one side of the scalp may be involved. The swelling may feel soft, firm or nodular when touched.
Recurrent attacks of granulomatous cheilitis may occur within days or even years after the first episode. At each episode, the swelling may become larger, more persistent and eventually become permanent. At this time the lips may crack, bleed and heal leaving a reddish-brown colour with scaling. This can be painful. Eventually, the lip takes on the consistency of hard rubber.



Other symptoms that may accompany granulomatous cheilitis include:
- Fever, headache and visual disturbances
- Mild enlargement of regional lymph nodes in 50% of cases
- Fissured or (pleat-like effect) tongue in 20–40% of cases
- Facial palsy; this can be intermittent, then possibly permanent and can be unilateral or bilateral, and partial or complete. It occurs in about 30% of cases of granulomatous cheilitis and indicates progression to orofacial granulomatosis.
TREATMENT:
If it is related to an allergy, responsible dietary components or causative substances should be avoided long-term. If there is an underlying disease, systemic treatment for this may also reduce the swelling of the lips.
The following measures have been reported to reduce the severity of granulomatous cheilitis in at least some cases.
- Topical corticosteroids
- Long term anti-inflammatory antibiotics, such as a six to twelve-month course of tetracycline, erythromycin or penicillin
- Intralesional corticosteroids injected into the lips to reduce swelling. Injections need to be repeated every few months.
- Non-steroidal anti-inflammatory agents
- Mast cell stabilizers such as ketotifen
- Clofazimine
- Sulfasalazine
- Surgical reduction
- DRUG INDUCED CHEILITIS
- Retinoid treatments (isotretinoin, acitretin, alitretinoin) may cause erythematous and squamous cheilitis that is dry and erosive with fissures. It correlates with a daily dose of treatment.
- Hemorrhagic crusting of the lips is a feature of Steven Johnson syndrome which is commonly caused by drugs but, cheilitis can occur as an isolated feature of a drug reaction- either as a result of allergy or a pharmacological effect.
3) CARCINOMA OF LIP:
Squamous cell carcinoma is the most common malignancy to affect the vermillion zone.
Lip cancer develops from abnormal cells that grow out of control and form lesions or tumors on the lips. Lip cancer is a type of oral cancer. It develops in thin, flat cells — called squamous cells.

SIGNS AND SYMPTOMS:
- a sore, lesion, blister, ulcer, or lump on the mouth that doesn’t go away
- a red or white patch on the lip
- bleeding or pain on the lips
- swelling of the jaw
- The patient may complain of difficulty in speech, difficulty in taking food and inability to close the mouth.
- There is also pain, bleeding and paraesthesia.
- Crater like lesion having velvety red base and rolled indurated borders.
Lip cancer may not have any symptoms. Dentists often first notice lip cancer during a routine dental exam. If you have a sore or lump on your lips, it doesn’t necessarily mean you have lip cancer, though. Discuss any symptoms with your dentist or doctor.
In untreated cases there is total destruction of lip and invasion of cheek, the gums and the mandible.
MANAGEMENT:
- Surgical: Prognosis is good if the treatment is done before metastasis
- The best results are seen when being obtained when the entire lip mucosal field is removed for early lesion.
PREVENTION:
Prevent lip cancer by avoiding the use of all types of tobacco, avoiding excessive alcohol use, and limiting exposure to both natural and artificial sunlight, particularly the use of tanning beds.
Many cases of lip cancer are first discovered by dentists. Because of this, it’s important to make regular dental appointments with a licensed professional, especially if you’re at an increased risk for lip cancers.
